The global spread of killer fungi is not just an issue for the UK. It’s a growing threat worldwide, one that could continue to worsen as climate change accelerates. With increasing global temperatures and erratic weather patterns, the ability of fungi to adapt and thrive in new environments is a serious concern for public health.
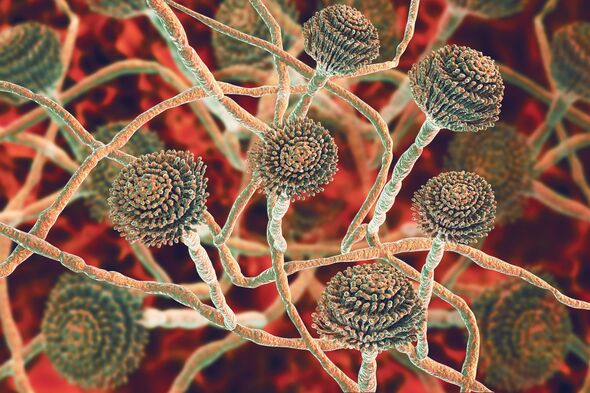
Fungi have long been a part of the natural world, playing essential roles in decomposition and nutrient cycling. However, their ability to cause infections, especially in immunocompromised individuals, has made them an emerging concern in the medical field. The fact that these organisms can be resistant to common antifungal treatments only adds to the difficulty of combating them. As new strains of fungi continue to emerge, health professionals and researchers are scrambling to stay one step ahead.
GLOBAL HOTSPOTS FOR FUNGAL INFECTIONS AND THEIR INCREASED PRESENCE IN THE UK
The expansion of killer fungi is particularly notable in countries that have seen significant climate changes. Tropical and subtropical regions have long been home to the most dangerous fungi, but as climate patterns shift, these regions are no longer the exclusive habitats for these pathogens. Areas once considered safe from such infections are now seeing increased fungal activity.
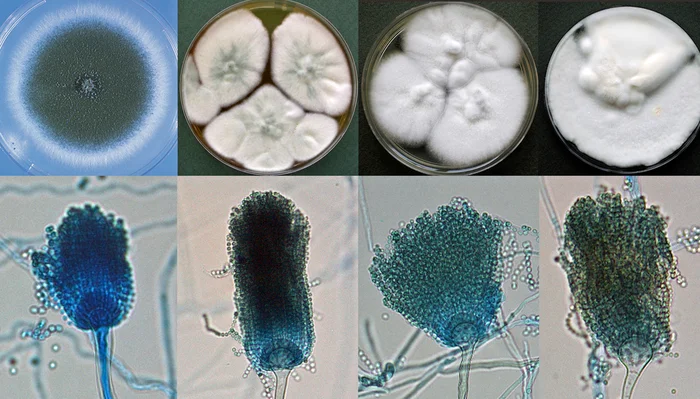
For example, the United States has already witnessed outbreaks of Candida auris in major cities, and several reports have indicated that the fungus is making its way across the world. In parts of Asia, particularly in India and Japan, the presence of Aspergillus fumigatus has increased dramatically due to changing weather conditions. The UK, typically associated with its cooler climate, may not have been as affected by these pathogens in the past. However, this is quickly changing.
As temperatures rise, fungi that were once limited to warmer climates are starting to spread more widely. This not only increases the risk of infections but also challenges the healthcare infrastructure in the UK, where climate change models predict higher humidity levels, particularly during the summer months. This is the perfect breeding ground for fungi that thrive in damp, warm environments.
THE SPREAD OF KILLER FUNGI THROUGH HOSPITALS AND HEALTHCARE SETTINGS
One of the most concerning aspects of the killer fungi threat is their ability to spread rapidly in hospital settings. Hospitals, by their very nature, are places where people with compromised immune systems are already at higher risk of infection. A fungus like Candida auris, which can survive on hospital surfaces for extended periods, poses a unique challenge.
Hospitals in the UK have already reported cases of Candida auris, and with an increasingly mobile global population, the risk of these fungi spreading more widely becomes even greater. Once a fungal infection takes hold in a healthcare setting, it can lead to widespread outbreaks, putting vulnerable patients at greater risk. This is particularly concerning in the context of the aging UK population, many of whom are already suffering from conditions that make them more susceptible to infections.
Moreover, the difficulty in diagnosing fungal infections only exacerbates the problem. Fungal infections often present symptoms similar to those of other more common illnesses, meaning they can easily be misdiagnosed, delaying the start of treatment. By the time a correct diagnosis is made, the infection could be much harder to treat, especially with the rise in antifungal resistance.
FUNGAL RESISTANCE AND THE LIMITATIONS OF ANTIFUNGAL MEDICATIONS
A key feature of many killer fungi is their growing resistance to existing antifungal drugs. This phenomenon, known as antifungal resistance, is making it increasingly difficult to treat infections caused by fungi like Candida auris and Aspergillus fumigatus. As the resistance of these pathogens grows, scientists and healthcare providers are faced with limited treatment options.
Antifungal drugs have long been a cornerstone of treating fungal infections, but resistance to these medications has been growing over the past few decades. This is partly due to overuse of antifungal drugs in both medical settings and agriculture, leading to the development of resistant fungal strains. The rise of antifungal-resistant strains of Candida auris and other fungi presents an urgent challenge for health systems around the world.
This situation underscores the need for new antifungal treatments, as well as better diagnostic tools that can quickly identify resistant strains. Researchers are actively exploring new ways to combat these pathogens, including the development of new drugs and innovative treatment strategies. However, these solutions may take time to come to fruition, and in the interim, public health systems must be prepared to deal with the rising threat of resistant fungal infections.
PREVENTION STRATEGIES: WHAT CAN BE DONE TO PROTECT AGAINST FUNGI?
Given the threat posed by killer fungi, it’s essential to adopt effective prevention strategies, especially in vulnerable settings like hospitals and healthcare facilities. In addition to improving infection control measures within hospitals, individuals can take steps to reduce their exposure to fungi in everyday life. These simple precautions can go a long way in preventing the spread of these dangerous pathogens.
- Hygiene Practices: Good hygiene is the first line of defense against fungal infections. Regular handwashing, especially after touching surfaces in public places, can help reduce the spread of fungal spores. Healthcare workers should take extra precautions to ensure that they are not spreading fungal spores between patients.
- Control of Environmental Factors: In places like hospitals, controlling the environment to minimize fungal growth is critical. Using air filtration systems, controlling humidity, and regularly cleaning surfaces with antifungal disinfectants can help reduce the presence of fungi in healthcare environments.
- Early Diagnosis and Surveillance: Surveillance and early detection are essential in the fight against fungal infections. Hospitals and healthcare providers should invest in systems that allow for the rapid identification of fungal infections, particularly those caused by resistant strains.
- Public Awareness Campaigns: Public health organizations should continue to raise awareness about the risks of fungal infections, especially in the context of climate change. Educating the public on the importance of hygiene and early detection can reduce the incidence of infections and prevent outbreaks.
- Research and Development: Finally, investment in research is crucial for developing new antifungal treatments and diagnostic tools. As fungi evolve to become more resistant to existing medications, the need for new therapies becomes even more urgent.
CLIMATE CHANGE AND THE FUTURE OF FUNGAL INFECTIONS IN THE UK
The future of fungal infections in the UK depends largely on how the climate continues to evolve. If current trends continue, the UK could see an increase in the number and severity of fungal outbreaks. Changes in temperature and humidity will create an environment where fungi like Candida auris and Aspergillus fumigatus can thrive.
However, climate change also offers an opportunity to address the issue before it becomes a full-blown public health crisis. By implementing strong climate mitigation measures, such as reducing greenhouse gas emissions and investing in green infrastructure, it may be possible to limit the extent of climate change and, by extension, reduce the spread of killer fungi. Additionally, proactive public health measures, including improved surveillance and better infection control practices, will be crucial in managing the growing threat of fungal infections.
CONCLUSION: TAKING IMMEDIATE ACTION AGAINST KILLER FUNGI
The threat of killer fungi is real, and as climate change accelerates, the risk to the UK and other countries grows. With the emergence of dangerous fungi like Candida auris and Aspergillus fumigatus, it’s essential for both individuals and healthcare systems to take action now to protect against the spread of these deadly pathogens. By improving hygiene, investing in new research, and preparing healthcare systems to deal with outbreaks, we can mitigate the impact of these infections.
In the fight against killer fungi, the clock is ticking. The sooner we act, the more likely we are to prevent a public health crisis in the future. As the climate continues to change, the time for complacency has passed. Immediate action is needed to safeguard the health of our populations and protect vulnerable individuals from the rising threat of killer fungi.